My son needed care, the system waited for a crime
By Anonymous in Texas
My son is a gentle and kind soul. When he is stable on his medication, he is my friend, and he always looks out for his family. He enjoys music and hiking and writes poetry, short stories, and song lyrics. Like many people with severe mental illness (SMI), he is capable of thriving with proper treatment. But the system isn’t built to help him thrive. Instead, he’s been ignored or treated like a dangerous criminal whenever his treatment needs have increased. He is currently doing well only because of my own costly efforts combined with a small bit of luck.
He was first diagnosed about seven years ago, after a series of difficult and confusing episodes. I learned about evidence-based treatments for schizophrenia, and I had so much hope! It seemed clear that with the right team of helpers, my son could live a successful life despite his disability. I learned the hard way that barriers were going to make those evidence-based treatments almost impossible to access, and I wouldn’t be able to intervene in his behalf when he most needed me.
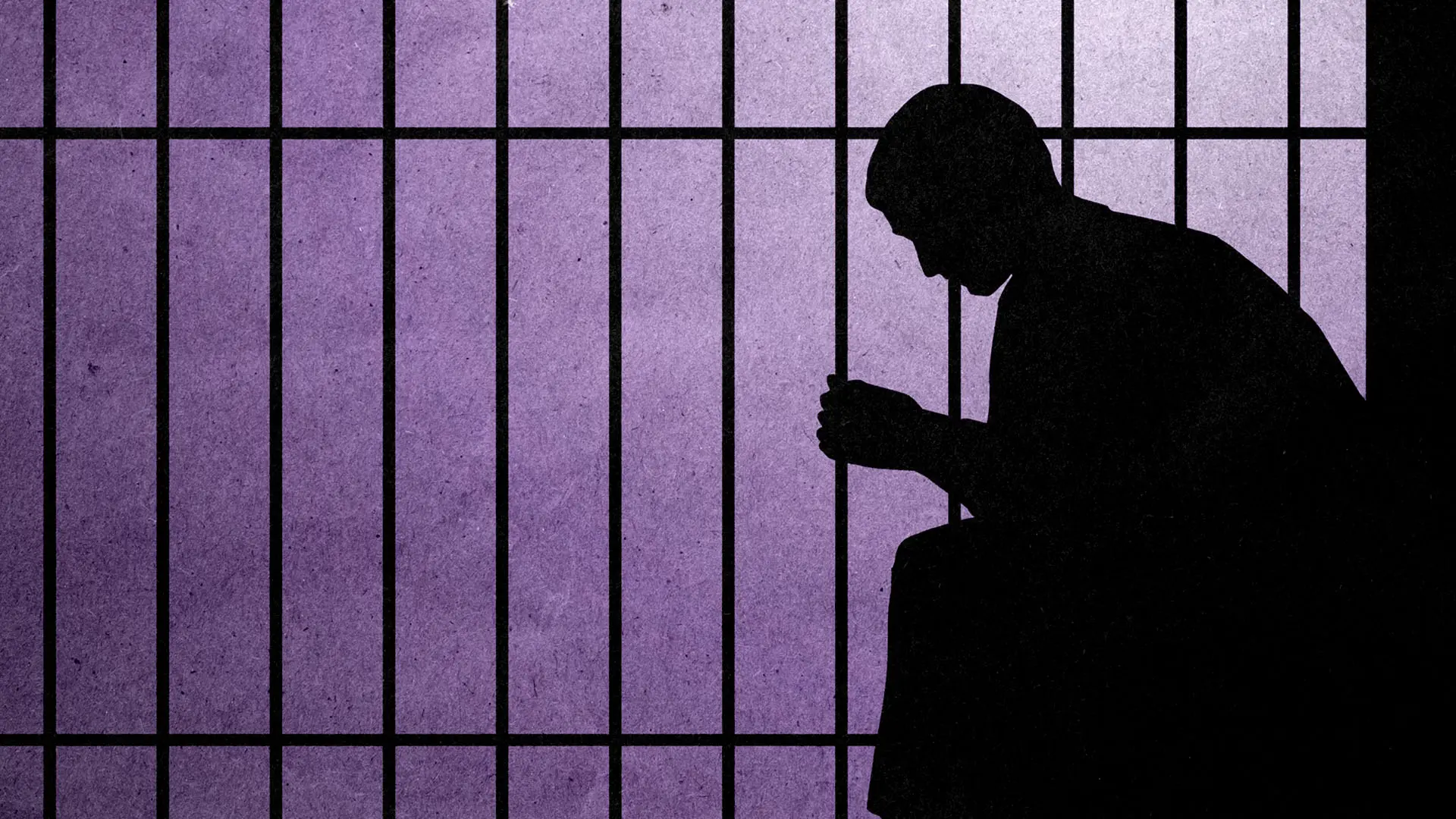
My son has been incarcerated four times during psychotic episodes. Each time, I have actively begged his providers to help him access an inpatient bed to re-stabilize. I have contacted the local crisis response service. I’ve taken him to the emergency department for an evaluation. Each time, every professional has told me that he’s not sick enough to warrant hospitalization. Each time he was found not dangerous enough until he met criteria to be arrested instead.
The most recent time this happened was in 2023. A few hours after the emergency department dismissed him, my son was involved in an accident. He was arrested and charged with vehicular assault that caused severe bodily injury. That met criteria for that elusive hospitalization, but he was of course incarcerated instead. While he was in jail, no one would provide any information about his legal status or his condition. His mental health team said they couldn’t do anything, now that he was justice involved.
I was desperate. I did not know whether my son was injured in the accident, if he was receiving any medical or mental health treatment. Because no one directly involved in his care would communicate with me, I wrote letters to my state elected officials and every news and radio outlet I could think of. I got no response from anyone. I was clearly the only one who felt any urgency. I found myself wondering what would have been different if my son had a stroke or was only injured in an accident. Would he and I be treated this way?
After about a month of no response from anyone who was supposed to care for my son, including his defense attorney, I hired a private attorney. This cost $10,000 I couldn’t afford, but I was able to negotiate a payment plan. Over six months, my son’s court hearings were postponed for a range of reasons until finally a court-appointed evaluator assessed him and concluded that he was fit enough to face his charges. My privately hired attorney recommended I hire an expert psychologist, costing me $2,000 (a discounted rate because they took pity on us after hearing my story). Meanwhile, I was visiting my son virtually (for a fee), as in-person visits were not allowed. His health was deteriorating quickly. He was withdrawn and had lost 100 pounds, down to a very unhealthy weight.
After reviewing the report from the psychologist I hired, the state-appointed psychologist changed their decision and found him unable to act in his own defense. After that, the case shifted toward a not guilty by reason of insanity plea and he was court-ordered into inpatient services at the state hospital. I had to pay nearly a thousand dollars in court fees.
Ultimately, it took almost two years and $15,000 for my son to get the inpatient care he had needed all along. While the state failed him, he experienced brain damage from untreated psychosis and tremendous trauma. I, too, have been severely traumatized, all because the requirement for medical care was “dangerousness,” not my son’s obvious need for treatment.
Before that illness episode, my son was working, taking care of his own activities of daily living, and talking about going back to college. Even when things were going well, we lived in fear that any decompensation would be devastating because each episode meant he had to lose everything all over again before getting the medical care he desperately needed. Once he was back in treatment, he came back to being his kind, loving self. Giving him back his chance at life didn’t need to cost so much — for our family or the state.